Do you ever have trouble recognizing a familiar face? I do from time to time. But frankly, I was surprised to know that there are individuals for whom this is beyond an occasional nuisance, and it profoundly affects their social and emotional lives because of a neurological condition called prosopagnosia.
I first heard of prosopagnosia when I was an undergraduate reading Oliver Sacks’ 1985 book, “The man who mistook his wife for a hat.“ Sacks shared the daily experiences of people living with prosopagnosia. The everyday difficulties that occur because of their inability to recognize familiar faces were astonishing. Imagine not being able to recognize your own spouse!
Edwin Burns*, Elizabeth Gaunt, Betiel Kidane*, Lucy Hunter*, and Jaylea Pulford (*pictured below) argue that we should reconsider common inclusion criteria in prosopagnosia research. They also explain how a simpler, faster diagnostic procedure could improve scientific and clinical outcomes in the field. Using the new diagnostic test, this condition may be more common than the typically reported 2-3%.
Reconsidering diagnostic procedures and research protocols could also help patients with difficulty recognizing familiar faces have better healthcare experiences than in the present. According to Burns,
“Medical gaslighting, where patients report ailments but are told by clinicians, they are perfectly fine, has gained huge public interest. Sadly, most people with prosopagnosia will experience this phenomenon because they will never acquire a diagnosis using current approaches. Instead, they are told that there is nothing wrong with them, that they simply don’t understand that their face recognition skills are intact, despite not recognizing partners, children and friends. In our paper we demonstrate a much more effective approach for diagnosing prosopagnosia, one we hope will enable every possible person suffering from this condition acquire a diagnosis. Moreover, our new method only takes a couple of minutes to administer, in contrast to previous approaches that took 20-30 minutes. Improving diagnosis accuracy should reduce patient distress and help those with prosopagnosia access support more easily.”****
A case for testing people classically excluded from prosopagnosia research
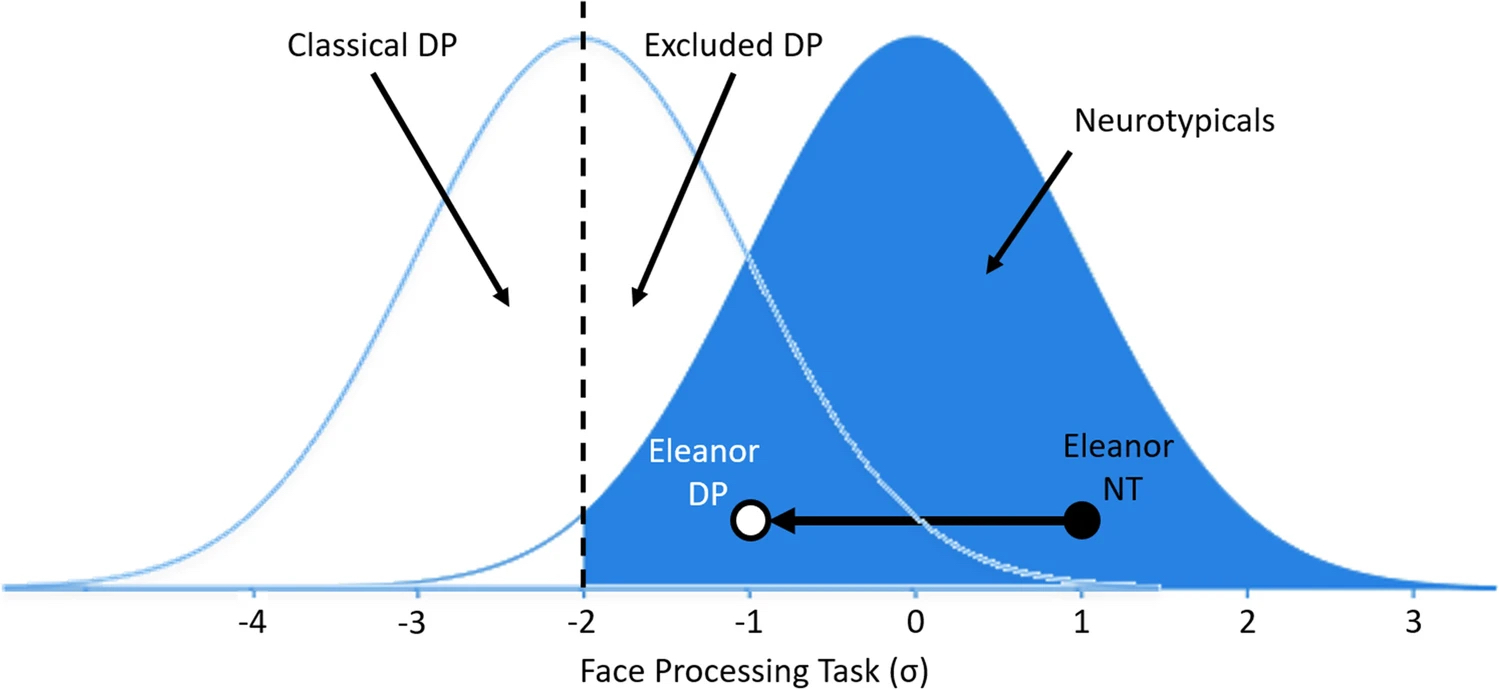
The authors note that due to a lack of clear guidance on diagnostic procedures for prosopagnosia, most research requires people with difficulties to recognize faces to perform more than ~2 standard deviations below the neurotypical mean. With this approach, more than 50% of people who believe they may have this condition fail to meet the inclusion criteria.
A key problem with this approach, the authors argue, is that if the threshold is so conservative (as shown in the figure below), but the distribution of performance impairments overlaps to an extent with the neurotypical population, a high ratio of true prosopagnosia cases is excluded from research and access to clinical care. This can lead to many drawbacks, a few of them being:
- Inaccurate prosopagnosia diagnoses. Because the baseline level of impairments in individuals with prosopagnosia is unknown, an excessively conservative threshold can fail to identify individuals with the condition (and lead to negative emotional and healthcare outcomes for individuals mistakenly considered neurotypical).
- Inaccurate estimates of the prevalence and performance distribution of prosopagnosia. If a considerable proportion of individuals with true prosopagnosia is excluded from research, the prevalence will be underestimated, and the performance distribution will be skewed (which would also inflate estimates of cognitive impairments).
- Undermining progress in treatment approaches. If treatments are only tested with individuals with prosopagnosia who perform at the lowest end of the distribution, the effectiveness of treatments may be underestimated (especially if individuals with milder impairments may be the ones who benefit the most from therapeutic options).
Including excluded cases: Are they different from individuals meeting classical criteria?
To put these ideas to the test, the authors recruited a large cohort of people experiencing difficulties recognizing faces and tested their facial recognition, memory, and perception. They also requested the individuals in their sample to self-rate the severity of their prosopagnosia-related symptoms.
They classified them as classical prosopagnosia patients (if they met traditional inclusion cutoffs) or excluded prosopagnosia cases (if they wouldn’t meet them) and compared their performance with that of a group of control participants.
The results showed many similarities between the classic and excluded prosopagnosia groups and differences from the control participants. The two findings that drew my attention the most were:
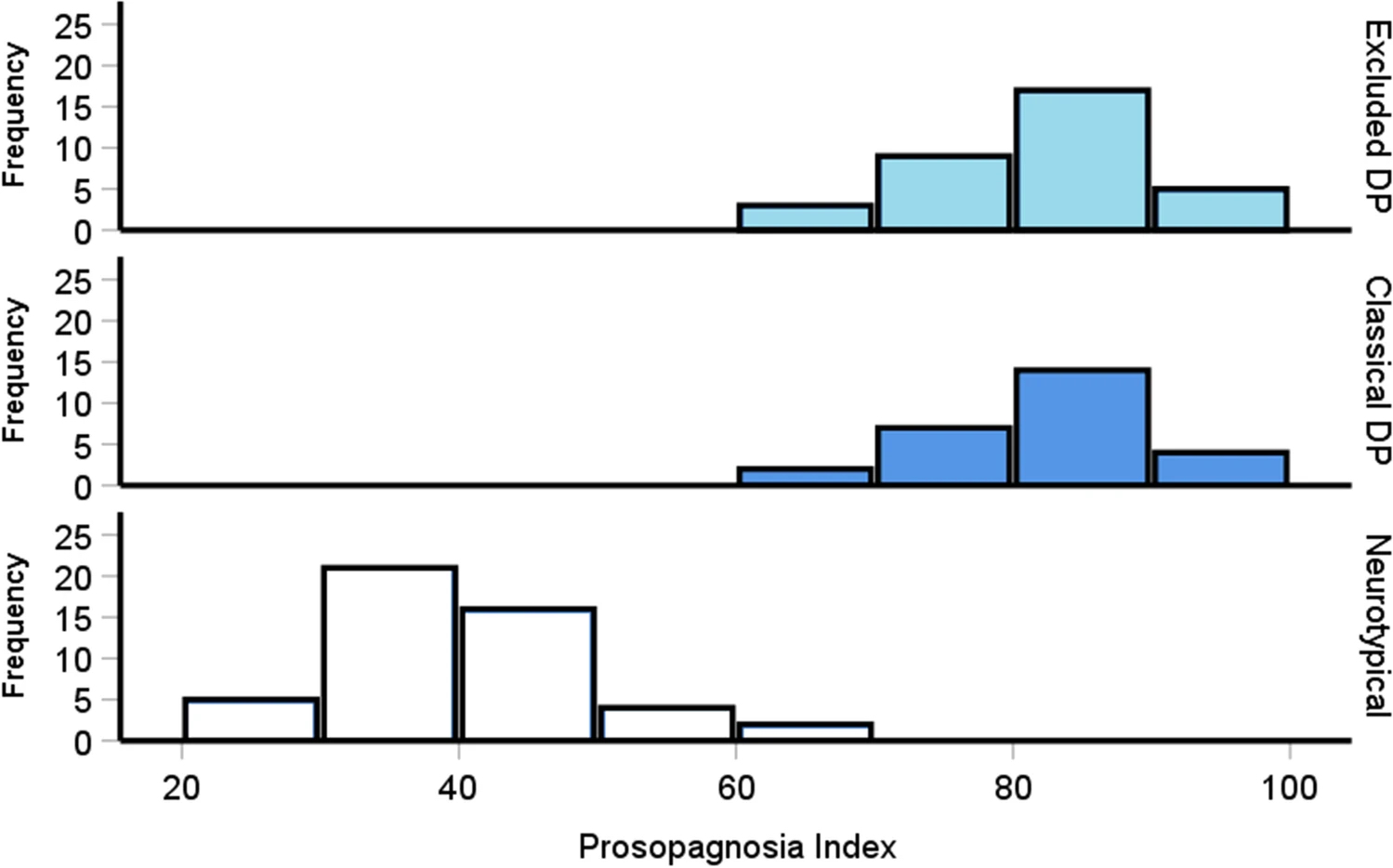
- The severity of symptoms of classical and excluded prosopagnosia participants was comparable to each other and higher than control participants, as shown in the plot below.
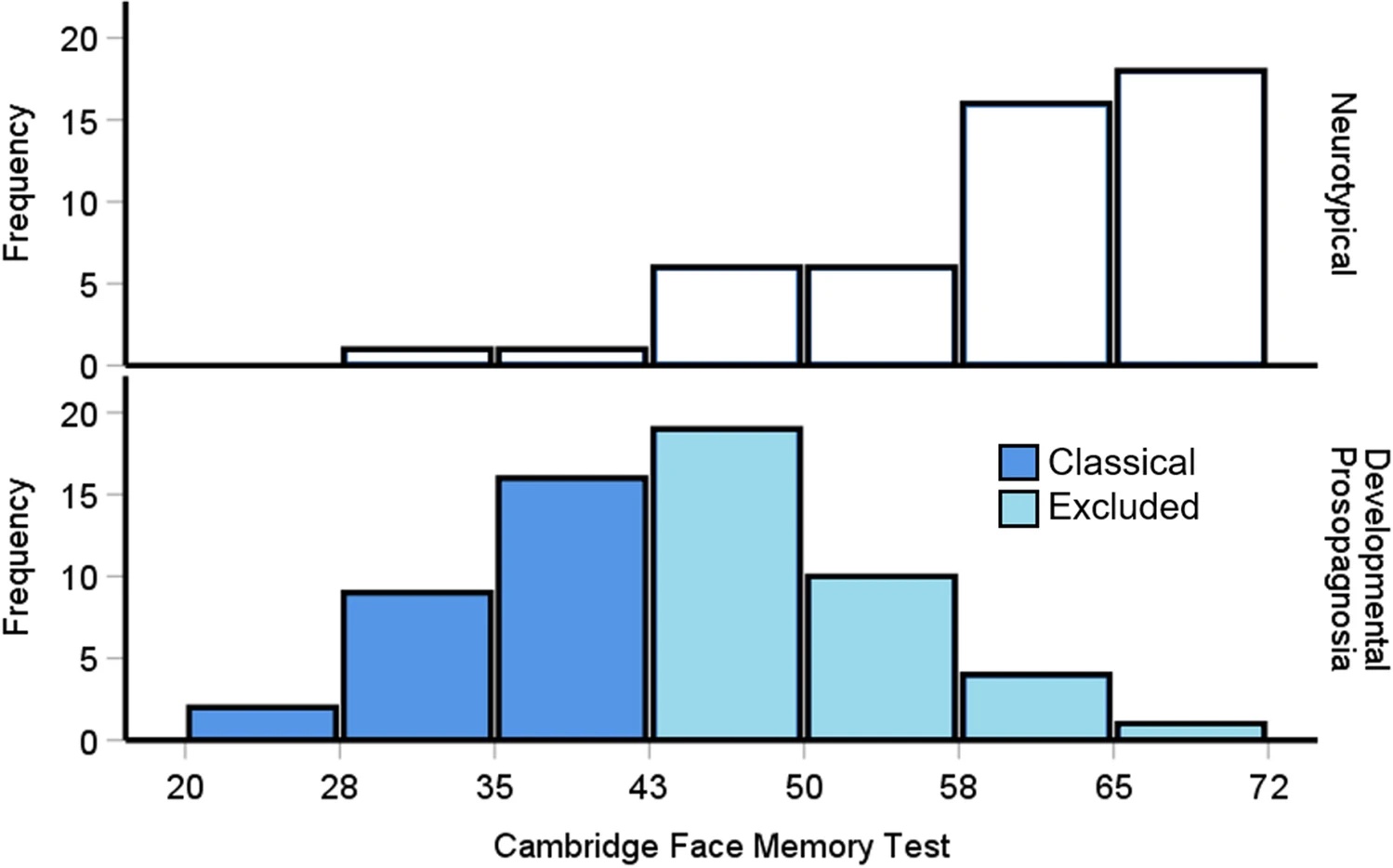
- The memory of Classical and Excluded prosopagnosia participants revealed impairments as compared with the control group. Moreover, the performance of classical and excluded individuals suggests a normal distribution when considered part of the same group, as shown in the plot below.
Sensible suggestions for researchers and clinicians
The classical approach, based on the Cambridge Face Memory Test, missed more than half of individuals who believe they have the condition. In comparison, an approach based on self-reporting symptoms (using the prosopagnosia index) virtually classified all of them correctly.
Because of this, the authors recommend basing the diagnosis of prosopagnosia and the inclusion of participants in scientific research on participants’ self-report of symptoms. This seems like a sensible suggestion, not only because it honors individuals’ lived experiences, but also results in a much faster approach (a couple of minutes vs 20+ minutes) and is much easier to administer and interpret.
One thing I really appreciated about the authors’ recommendations is that they also honor the experiences and constraints that researchers face. Acknowledging the pressing need for novel results in scientific research, and the tendency to prefer a conservative threshold when making empirical claims, the authors recommend performing primary analyses using classical inclusion criteria thresholds, and reporting additional analyses including classically excluded prosopagnosia cases.
This approach, they argue, would allow researchers not to lose any novelty or scientific rigor. At the same time, it can serve as an empirical test on whether the cognitive characteristics of classical and excluded prosopagnosia individuals differ or can be considered as belonging to the same underlying distribution.
In other words, with a more accurate way to diagnose it, we can better understand how common it is, how it affects people’s lives, and how clinicians can help them.
Featured Psychonomic Society article
Burns, E.J., Gaunt, E., Kidane, B., Kidane, B., Hunter, L., & Pullford, J. (2022). A new approach to diagnosing and researching developmental prosopagnosia: Excluded cases are impaired too. Behavior Research Methods. https://doi.org/10.3758/s13428-022-02017-w
****Read more about this topic in “A new approach to diagnosing and researching developmental prosopagnosia: Excluded cases are impaired too”, published in Behavior Research Methods, a journal of the Psychonomic Society.
